- 3120 Fire Road, Suite 201 Egg Harbor Township, NJ 08234
- 888-564-6152
Note: The information listed may change and update as the situation unfolds. Visit New Jersey’s COVID Information site here.
NEW: “Where And When Can I Get The COVID-19 Vaccine?”
As states roll out their vaccination plans, a common question we keep hearing is, “Where and when can I get the COVID-19 vaccine?” Each state is handling the vaccine distribution differently. Find out if you’re eligible yet by clicking here.
New Jersey Vaccine Scheduling System (NJVSS)
 The New Jersey Department of Health has recently launched the NJ Vaccine Scheduling System (NJVSS), a system where individuals can pre-register for the COVID-19 vaccine!
The New Jersey Department of Health has recently launched the NJ Vaccine Scheduling System (NJVSS), a system where individuals can pre-register for the COVID-19 vaccine!
COVID-19 vaccines are on the way to hospitals and clinics across New Jersey. Residents can pre-register to reserve a spot to get a vaccine now by clicking here.
Pennsylvania Launches “Your Turn” Quiz
 The Pennsylvania Department of Health has created a new quiz called “Your Turn” to determine each resident’s eligibility to receive the COVID-19 vaccine.
The Pennsylvania Department of Health has created a new quiz called “Your Turn” to determine each resident’s eligibility to receive the COVID-19 vaccine.
If it is your turn, you will be directed on how to find a vaccine provider. Click here to get started.
*Note: If you plan to get vaccinated in Philadelphia County, please note that Philadelphia County is a separate vaccine jurisdiction and has its own information about vaccine distribution.
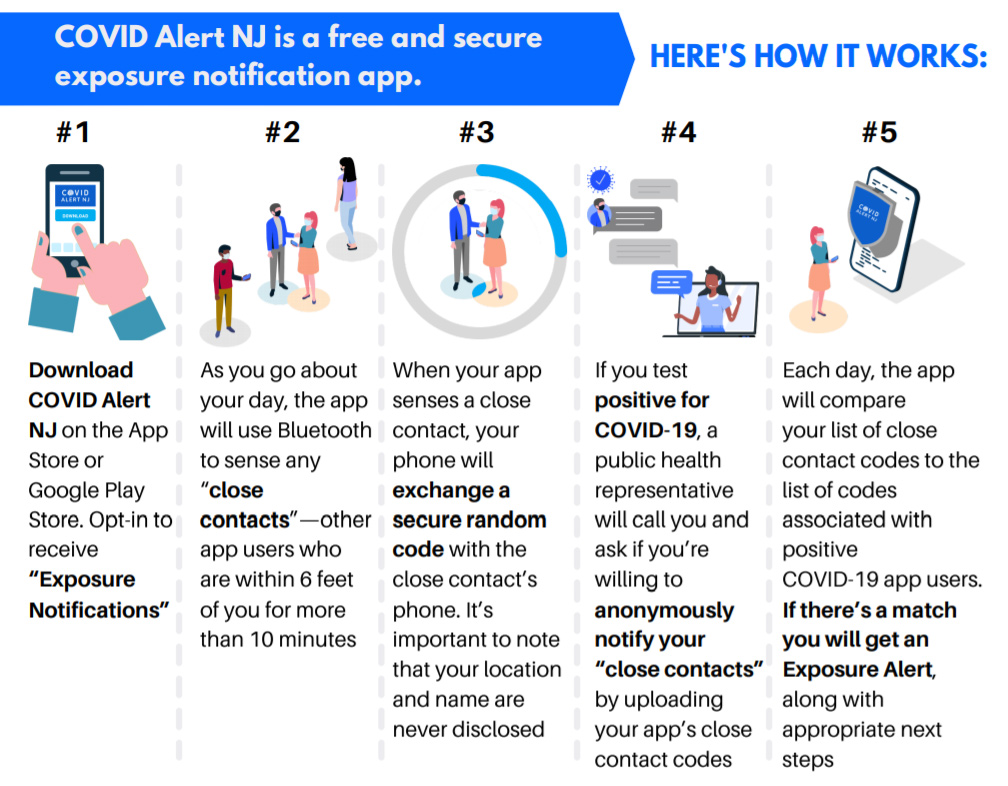
“COVID Alert NJ” App
In early October, the New Jersey Department of Health announced the launch of “COVID Alert NJ,” a new app available on the Google Play Store and Apple App Store for free. This app will be a crucial public health tool in keeping workers and patrons safe and allowing businesses to stay open!
We encourage our members to use this new app to protect themselves and their families from exposure. Learn more and download the app on NJ.gov!
Pennsylvania and Delaware also have similar apps available for download: COVID Alert PA and COVID Alert DE.
Protection for Workers
Healthcare Workers
The UFCW recommends that all potentially exposed healthcare workers have access to adequate supplies of N95 disposable, filtering facepiece respirators, which are commonly used in healthcare. Some employers have begun using respirators, such as elastomeric half-masks and Powered Air-Purifying Respirators (PAPRs), which are even more protective than N95 respirators. Personal protective equipment also includes gloves, gown, and a face shield.
OSHA requires the employer to fit test workers annually, as well as when the worker has experienced significant weight fluctuation, dental work or other facial differences that would impact the seal of a tight-fitting respirator. PAPRs use hoods and do not require fit testing. Workers must be medically cleared to use respirators. All workers are entitled to training on respirator use. Surgical masks are never adequate for respiratory protection.
Workers responsible for cleaning patient rooms, treatment rooms, and equipment must be provided appropriate PPE and training to protect them both from contracting the coronavirus and from the strong chemicals used to kill the virus. If the employer introduces new cleaning products into the facility, the workers are entitled to training on the product, as required by OSHA’s Hazard Communication Standard.
CDC recommends the following protocols for Infection Control Procedures in healthcare settings:
Patients with suspected coronavirus should be given a surgical mask and moved immediately into an isolation room, preferably a negative pressure room. The facility’s infection control plan should provide guidance on isolation, cleaning, sanitizing, and sterilization of patient care equipment.
All personnel who enter the patient’s room should use standard, contact and airborne precautions—gowns, gloves, face shields and NIOSH-certified disposable N95 or stronger respirators, such as powered air-purifying respirators (PAPRs). Surgical masks are not a substitute for respirators and do not protect the wearer. Donning personal protective equipment (PPE) should be done in the following order:
- Wash or gel hands
- Gown
- Respirator
- Face shield or goggles
- Gloves
When removing or doffing PPE, the user should assume the exterior is contaminated. Doffing PPE should be done in this order:
- Gloves
- Eye cover
- Gown
- Respirator
- Wash or gel hands
There should also be a facility protocol to evaluate workers who report fevers and symptoms after exposure to a suspected and/or confirmed infected patient. Employers should keep records of any worker infection, which should be investigated and presumed to be work-related unless proven otherwise.
Retail Workers
As a grocery or food retail worker, potential sources of exposure include close contact for prolonged periods of time with a customer with COVID-19 and touching your nose, mouth, or eyes after handling items, cash, or merchandise that customers with COVID-19 have touched.
- Workers should have access to adequate supplies of alcohol-based hand sanitizers at the workstation as well as disinfectants to clean and disinfect workstations.
- Frequently wipe down the workstation with disinfectant.
- Take frequent breaks to wash hands with soap and water for at least 20 seconds.
- Avoid touching your eyes, nose, and mouth with unwashed hands
- Stay home from work if you exhibit symptoms of acute respiratory illness such as coughing or shortness of breath.
For more information on the CDC guidelines for retail workers, visit their website here.
Food Processing Workers
Workers in food processing plants work in close proximity to other workers. The manufacturing work environment—production or assembly lines and other areas in busy plants where workers have close contact with coworkers and supervisors—may contribute substantially to workers’ potential exposures.
- Clean your hands often with an alcohol-based hand sanitizer that contains at least 60-95% alcohol or wash your hands with soap and water for at least 20 seconds. Soap and water should be used preferentially if hands are visibly dirty.
- There should be adequate supplies of soap and water in bathrooms, and alcohol-based hand sanitizers in the workplace.
- Avoid touching your eyes, nose, and mouth with unwashed hands.
- Personal protective equipment, such as gloves, should be replaced on a regular basis.
For more information on the CDC guidelines for food processing and manufacturing plant workers, click here.
Priorities for the UFCW for all industry sectors:
UFCW Local 152 is encouraging employers to have the following in place:
- Comprehensive workplace plans to identify potential exposure routes, controls to mitigate risk and training procedures.
- Protections for different groups of workers, following the Occupational Safety and Health Administration guidelines.
- Policies to encourage sick workers to stay at home without the loss of pay, benefits, seniority or other benefits.
- Economic policies for unemployment scenarios, where people are not able to be at work or are required to work overtime to take care of patients.
- Emphasis on personal hygiene practices, hand-washing, and respiratory etiquette.
- Adequate supplies of personal protective equipment, especially N95 respirators, and respirator fit testing for highest at-risk worker, i.e. health care workers
- Protocols to clean and disinfect frequently touched objects and surfaces.
- Protocols in case of a workplace or community outbreak, including possible self-quarantine or workplace quarantine.
- Plans for supply shortages, triage, prioritization, and other contingencies.
- Consult the Centers for Disease Control and Prevention (CDC) before hosting and attending events or large gatherings. CDC recommendations may change as the situation evolves.
Emergency Child Care (NJ)
A few months ago, New Jersey launched an Emergency Child Care Assistance Program (ECCAP) to help support child care costs when a parent/guardian is an essential employee. This program is now closed.
However, if you still need help paying for child care, you can still apply for the state’s Child Care Subsidy Program.
For school-aged children, New Jersey is now offering a new program called School-Age Tuition Assistance Program, which will provide tuition assistance to parents/caretakers with school-age children (5 to 13 years old) in need of child care due to schools’ remote learning schedules this fall as a result of the COVID-19 public health emergency.
Unemployment FAQs (NJ)
New Jersey Department of Labor & Workforce Development
North New Jersey: 201-601-4100;
Central New Jersey: 732-761-2020;
South New Jersey: 856-507-2340;
Out of state: 888-795-6672
- Who qualifies for unemployment?
Most people who were employed for at least 20 weeks in the past year will qualify for unemployment, but there are some exceptions. See this website for details that may apply to your situation. - When should I file for unemployment?
You should file as soon as possible. You can file online or by phone, but you must file your claim at a certain time of day depending on the last four digits of your Social Security Number. Here are some additional instructions. - What if I don’t live and work in the same state?
You should file for unemployment in the state where you work. - What percentage of my pay will be replaced by unemployment benefits?
Your benefit rate is 60% of the average weekly wage you earned during the past year, up to the current maximum weekly benefit rate of $731. For a personalized estimate of the benefits you will receive, use the New Jersey State Department of Labor & Workforce Development’s benefit rate calculator tool. - What if I didn’t lose my job but am being scheduled to work fewer hours?
You can still apply for unemployment. You will likely receive at least partial unemployment benefits if you are working part-time when you usually work full-time. - I have a different question about unemployment benefits.
Check out the state’s FAQ page, or you can look at this chart for additional guidance. - What kind of paid sick leave or paid family leave do I get under the new federal law?
The new federal law requires your employer to provide 14 days of paid leave if you have coronavirus or if you are placed in quarantine to care for a family member who has coronavirus. You must receive at least two-thirds of your wages during that 14-day period. - I have another question!
See if it is already answered on New Jersey’s Department of Labor FAQs During Coronavirus.
Protecting Yourself
According to WHO and the CDC, the best way to prevent illness is to take preventative actions, such as:
- Wash your hands often with soap and water for at least 20 seconds, especially after going to the bathroom; before eating; and after blowing your nose, coughing, or sneezing.
- If soap and water are not readily available, use an alcohol-based hand sanitizer with at least 60% alcohol. Always wash hands with soap and water if hands are visibly dirty.
- Cover your mouth and nose with your elbow or a tissue when you cough or sneeze.
- Avoid touching your eyes, nose, and mouth if your hands aren’t clean.
- Avoid close contact with anyone who is sick.
- Clean surfaces you often touch.
- Stay home from work, school, and public areas if you’re sick.
Use of Cloth Face Coverings to Help Slow the Spread
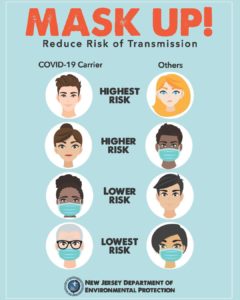 We now know from recent studies that a significant portion of individuals with coronavirus lack symptoms (“asymptomatic”) and that even those who eventually develop symptoms (“pre-symptomatic”) can transmit the virus to others before showing symptoms. The CDC recommends wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain (e.g., grocery stores and pharmacies) especially in areas of significant community-based transmission.
We now know from recent studies that a significant portion of individuals with coronavirus lack symptoms (“asymptomatic”) and that even those who eventually develop symptoms (“pre-symptomatic”) can transmit the virus to others before showing symptoms. The CDC recommends wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain (e.g., grocery stores and pharmacies) especially in areas of significant community-based transmission.
It is critical to emphasize that maintaining 6-feet social distancing remains important to slow the spread of the virus.
The cloth face coverings recommended are not surgical masks or N-95 respirators. Those are critical supplies that must continue to be reserved for healthcare workers and other medical first responders, as recommended by current CDC guidance.
STAY CONNECTED
MORE INFORMATION
U.S. Occupational Safety and Health Administration: osha.gov/SLTC/covid-19/index.html
- Centers for Disease Control and Prevention: cdc.gov/coronavirus/2019-nCoV/index.html
- https://emergency.cdc.gov/han/2020/han00428.asp
- World Health Organization: who.int/emergencies/diseases/novel-coronavirus-2019
Additional Guidance and Resources
Official State Health Departments
- State of New Jersey Department of Health – Coronavirus
- Pennsylvania Department of Health – Coronavirus
- Delaware Health and Social Services – Coronavirus
- Maryland Department of Health – Coronavirus